WHO Africa finalises validation for stronger and harmonised health workforce training
The World Health Organization Regional Office for Africa (WHO/AFRO) has finalised validation for African countries to adopt a unified and competency-based approach to training health professionals.
According to the Health Workforce Team Lead at the WHO Regional Office for Africa, Dr James Avoka Asamani, the initiative — known as the Africa Health Workforce Transformation and Harmonisation drive — aims to improve the quality and trustworthiness of health education across the continent.
Dr Asamani explained that the effort focuses on developing competency-based curricula, establishing robust accreditation frameworks, and implementing benchmarking mechanisms to standardise health training institutions.
“By developing competency-based curricula, instituting robust accreditation frameworks, and establishing benchmarking mechanisms, we are laying the foundation for harmonisation that will ensure trusted, high-quality health professions education across Africa,” Dr Asamani said.
Progress and persistent challenges
Over the last decade, the African region has made significant progress in expanding its health workforce. Between 2013 and 2022, the number of health workers tripled from 1.6 million to 5.1 million, including more than 800,000 community health workers. This reflects strong investments and a growing commitment to closing long-standing workforce gaps.
Despite this growth, the region still faces a projected needs-based shortage of 6.1 million health workers by 2030. Recent assessments also show that nearly 60% of health workers struggle with diagnostic and treatment accuracy, revealing major gaps in the quality of training and continuous professional development.
The region also faces both shortages and unemployment among health workers, with about 27% currently unemployed. The imbalance is intensified by high migration rates, as available figures show that one in ten African health workers is employed abroad, and more than 40% of those remaining have expressed intentions to migrate.
Multiple commitments and initiatives are underway to strengthen and integrate Africa’s health workforce. However, sustainable progress depends on foundational reforms in health professions education. Central to this is the adoption of competency-based education, supported by harmonised Health Professions Education Quality Standards that will enable reciprocal recognition of qualifications.
These reforms will improve the quality and relevance of health education and promote labour market integration across the continent.
The ongoing curriculum initiative represents a critical first pillar within the broader Africa Regional Health Workforce Harmonisation Programme, a five-step process designed to ensure quality, comparability, and cross-border mobility of health workers.
Developing Competency-Based Curricula
The Africa Prototype Competency-Based Curricula (CBC) will serve as reference models for countries to adapt, implement, and institutionalise competency-based education. The initiative reinforces WHO/AFRO’s commitment to supporting Member States in strengthening health systems and achieving UHC.
The curriculum development process was initiated during the Inaugural Africa Health Professions Education Dialogue held in Lusaka, Zambia, in 2024. During this dialogue, senior experts and leaders from various health professions, disciplines, and organisations reached a consensus on the key outcomes needed for priority health professions to effectively address the health systems’ needs in the African region.
These agreed outcomes became the foundation for the Competency-Based Curriculum (CBC) development. To date, seven consultants have been appointed to develop the regional prototype CBCs for 10 priority health professions.
The draft curricula were shared with more than 300 stakeholders, including academic institutions, professional associations, and health experts across Africa and beyond, for high-level review and feedback. The valuable comments from these stakeholders have since been incorporated into the final version.
The new curricula aim to close the competency gaps that exist among health workers in Africa. According to recent assessments, health workers on the continent correctly make only 60% of clinical diagnoses and 35% of treatments compared with standard medical guidelines.
For years, health professions education in Africa has struggled with limited resources, outdated curricula, and a shortage of qualified educators. These challenges have weakened the readiness of graduates to meet the health needs of their communities and patients.

Building on the Global Competency and Outcomes Framework for Universal Health Coverage (2022), the 10 curricula were co-created through a regional consensus process. A Curriculum Development Advisory Group – comprising experts in health professions education, health practitioners, policymakers, regulators, and professional associations—provided technical oversight to the process.
Validation, launch and expected outcomes
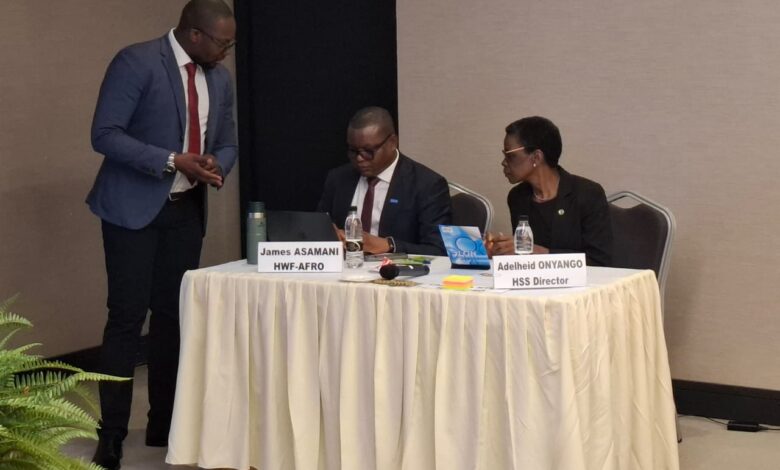
A total of 25 experts from 12 countries met in Kintele, Congo, from 7–9 October 2025 to finalise the curricula. The meeting, officially opened by Acting Director of the Health Systems and Services (HSS) Cluster at the WHO Regional Office for Africa, Dr Adelheid Onyango, brought together academics, regulators, professional associations, and partner organisations from across the continent.
The validated curricula are expected to be formally launched in November 2025 by the WHO Regional Director for Africa, Dr Mohamed Yakub Janabi.
WHO/AFRO says the initiative represents a major milestone toward creating a more skilled, trusted, and mobile health workforce that can respond effectively to Africa’s health priorities.
Dr. Onyango said the adoption of competency-based curricula marks a transformative investment in Africa’s health workforce.
“By equipping graduates with the skills, attitudes, and values needed to address the health realities of our populations, we are building a foundation for stronger, more resilient health systems”, she stated in her opening remarks.
The working session produced ten finalised regional prototype competency-based curriculum drafts for the following key occupations: Advanced Midwifery and Women’s Health, Basic Medical Education, Paediatrics and Child Care Nursing, Paediatrics and Child Health Medicine, AND Surgery
The rest include Obstetrics and Gynaecology, Critical Care Nursing, Health Information Systems, Community Health Workers and Emergency Nursing.
DISCLAIMER: The Views, Comments, Opinions, Contributions and Statements made by Readers and Contributors on this platform do not necessarily represent the views or policy of Multimedia Group Limited.
DISCLAIMER: The Views, Comments, Opinions, Contributions and Statements made by Readers and Contributors on this platform do not necessarily represent the views or policy of Multimedia Group Limited.
Source link